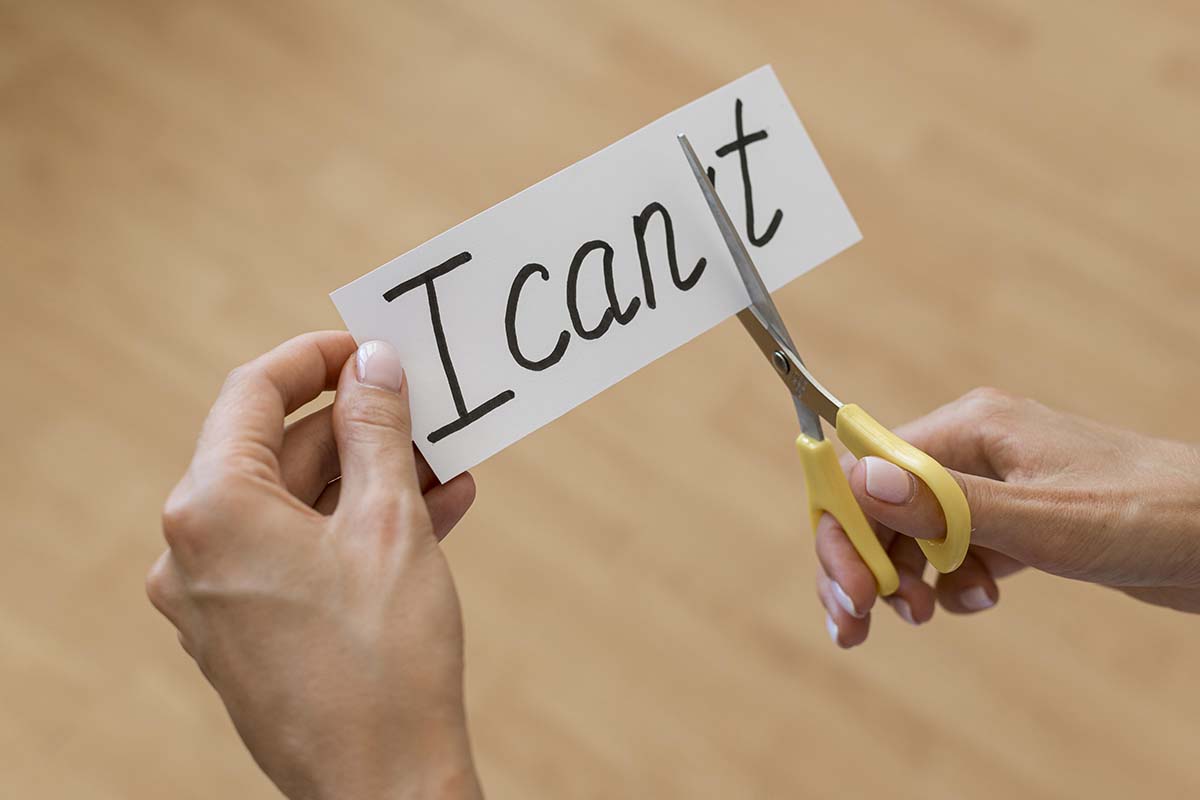
Why You Can’t Just Quit on Willpower Alone — and Why That’s Okay
✨Key Points
Addiction isn’t about weakness — it’s biology. Repeated substance use changes the brain’s chemistry, making “just stopping” nearly impossible without help.
Trying alone makes recovery harder. Isolation increases shame and relapse risk. Real healing happens through connection and professional support.
Recovery takes more than willpower. Medical care, therapy, and community address the physical, emotional, and psychological roots of addiction.
You’ve promised yourself a hundred times.
Tonight’s the last time. Tomorrow morning, things will be different. You’ll get it together.
You’ll prove to yourself — and maybe to the people who are starting to notice — that you have control over this.
And maybe you make it a day. Sometimes two. Once, you even made it a whole week, and for those seven days, you felt like yourself again.
Like the person you used to be before everything got so complicated.
But then it happens again.
The drink. The pill. The thing you swore you were done with.
And suddenly you’re right back where you started, except now there’s something new layered on top of everything else: shame. Deep, crushing shame that whispers you’re weak.
That if you really wanted to stop, you would.
That other people can handle their lives, so why can’t you?
✨Here’s what I need you to hear: The fact that you can’t just stop on your own doesn’t mean you’re broken. It means you’re human, and you’re dealing with something that was never designed to be overcome through willpower alone.
The Myth of “Just Stop”
We live in a culture obsessed with self-control.
We celebrate people who “pull themselves up by their bootstraps” and shame those who struggle.
Everywhere you look, there’s another story about someone who quit cold turkey, who just decided one day they were done and never looked back.
Those stories are real. But they’re also rare.
And they leave out a crucial detail: what was happening in that person’s brain, body, and life that made quitting possible for them in that moment.
For most people struggling with substance use, the idea of “just stopping” isn’t just difficult — it’s neurologically incomplete.
It’s like telling someone with a broken leg to just walk it off. The intention might be there.
The desire might be desperate and real. But something fundamental has changed in the way your brain and body function, and no amount of wanting it badly enough can override that on its own.
Your Brain Isn’t Betraying You — It’s Trying to Survive
When you use substances repeatedly, your brain adapts. It’s not being stubborn or weak — it’s actually doing exactly what it’s designed to do: learn patterns and optimize for survival.
Your brain has a reward system that lights up when you experience pleasure or relief.
Food, connection, accomplishment — these things activate it naturally.
But substances hijack this system, flooding it with dopamine levels far beyond what any natural reward could provide.
Over time, your brain recalibrates. It starts to expect those artificial highs and lows.
It restructures its chemistry around them.
This isn’t a character flaw. This is neurobiology.
When you try to stop suddenly, your brain doesn’t just miss the substance — it genuinely believes something is wrong.
It sends out distress signals. It creates cravings that feel as urgent as hunger or thirst.
It convinces you that you need this thing to function, to feel normal, to survive.
And here’s the part that makes it even harder: the areas of your brain responsible for decision-making, impulse control, and long-term planning?
Those get compromised too. So at the exact moment when you need your willpower most, the part of your brain that generates willpower is working at half capacity.
You’re not weak for struggling against this. You’re fighting your own biology.
And that’s a fight almost no one can win alone.
Leading experts at Serenity Malibu help individuals understand that addiction is a medical condition, not a moral failing, and that recovery requires addressing the neurological changes that have occurred through comprehensive, evidence-based treatment.
The Weight of Doing It in Secret
There’s another reason stopping on your own is so hard, and it has nothing to do with brain chemistry: isolation.
Maybe you’ve been managing this in private for months or years.
Maybe you’ve gotten really good at hiding it — showing up to work, taking care of responsibilities, maintaining the appearance that everything’s fine.
From the outside, you might look like you have it together.
But inside, you’re exhausted.
You’re carrying the weight of a secret that grows heavier every day.
You’re constantly calculating: How much can I use without anyone noticing?
How do I explain why I seem off?
What excuse can I give for canceling plans again?
And when you try to quit on your own, you’re doing it in that same isolation.
No one knows you’re trying. No one can support you through the hard moments.
When the cravings hit at 2 a.m. or during a stressful afternoon, you’re white-knuckling it alone, hoping sheer determination will be enough.
Sometimes it is. For a day, or three days, or even a week.
But sustainable change rarely happens in isolation. Human beings aren’t wired that way.
We heal in connection, not in hiding.
When “Just Stopping” Becomes Dangerous
Here’s something most people don’t realize: for some substances, trying to quit cold turkey on your own isn’t just difficult — it can actually be dangerous.
Alcohol and benzodiazepines, in particular, can cause life-threatening withdrawal symptoms.
Seizures, severe anxiety, delirium tremens — these aren’t just uncomfortable.
They can be medically serious. People have died from untreated withdrawal.
Even with other substances, the physical and psychological symptoms of withdrawal can be so overwhelming that relapse becomes almost inevitable.
Insomnia, nausea, anxiety, depression, cravings that feel like they’re consuming you from the inside out — when you’re experiencing all of that alone, getting through even one day can feel impossible.
This is why medical supervision during detox isn’t a luxury or a sign of weakness.
It’s often a medical necessity. It’s what allows your body to safely reset while professionals manage symptoms, provide support, and keep you stable.
The Shame Spiral That Keeps You Stuck
Every time you try to stop and can’t, the shame gets a little bit deeper.
You start to believe the story that you’re uniquely broken.
That other people could do this, but you can’t.
That you’ve proven you don’t have what it takes.
And that shame becomes its own trap.
Because when you feel terrible about yourself, the thing you’re struggling with becomes even more appealing.
It’s the thing that quiets the voice telling you you’re not enough. It’s the thing that provides temporary relief from the pain of feeling like a failure.
So you use again, which creates more shame, which makes you want to use again.
The cycle reinforces itself.
Breaking free from this isn’t about having more willpower or wanting it badly enough.
It’s about interrupting the cycle in a way that addresses all the layers — the physical dependence, the psychological patterns, the shame, the isolation, the underlying reasons you started using in the first place.
Leading experts at Serenity Malibu help clients break this cycle through trauma-informed care that addresses both the addiction itself and the emotional wounds that fuel it, creating a path forward that’s built on healing rather than willpower alone.
What Actually Makes Change Possible
If willpower alone isn’t enough, what is?
The answer is different for everyone, but it usually includes several elements working together: medical support to safely manage withdrawal, therapy to understand and address underlying causes, connection with others who understand what you’re going through, time and space away from the triggers and stressors of everyday life, new tools and strategies for managing emotions and cravings, and treatment of any co-occurring mental health conditions that might be fueling the cycle.
You can’t think your way out of a problem that involves your brain chemistry, your nervous system, your trauma history, and your environment all at once. You need an approach that addresses all of those things simultaneously.
That’s not weakness. That’s wisdom.
You’re Not Alone in This
If you’ve tried to stop on your own and couldn’t, you’re in the majority.
Most people who achieve lasting recovery don’t do it through willpower alone.
They do it with support, with professional help, with time, and with an approach designed around how addiction actually works.
The fact that you’ve tried — even if you’ve “failed” — means you haven’t given up.
It means some part of you is still fighting for the life you want.
That part of you, the part that keeps trying even when it feels hopeless, is stronger than you realize.
But it doesn’t have to fight alone anymore.
Getting help isn’t admitting defeat.
It’s choosing a strategy that actually matches the problem you’re facing.
It’s recognizing that you’re dealing with something complex and powerful, and meeting it with an equally comprehensive response.
You deserve support that actually works. You deserve treatment that addresses not just the substance use, but the pain underneath it.
You deserve to stop carrying this alone.
Because here’s the truth: you can’t always just stop on your own.
But that doesn’t mean you can’t stop at all.
It just means you need something more than willpower.
And that something exists. It’s available. And it works.