OCD and Linked Mental Health Disorders
✨Key Points
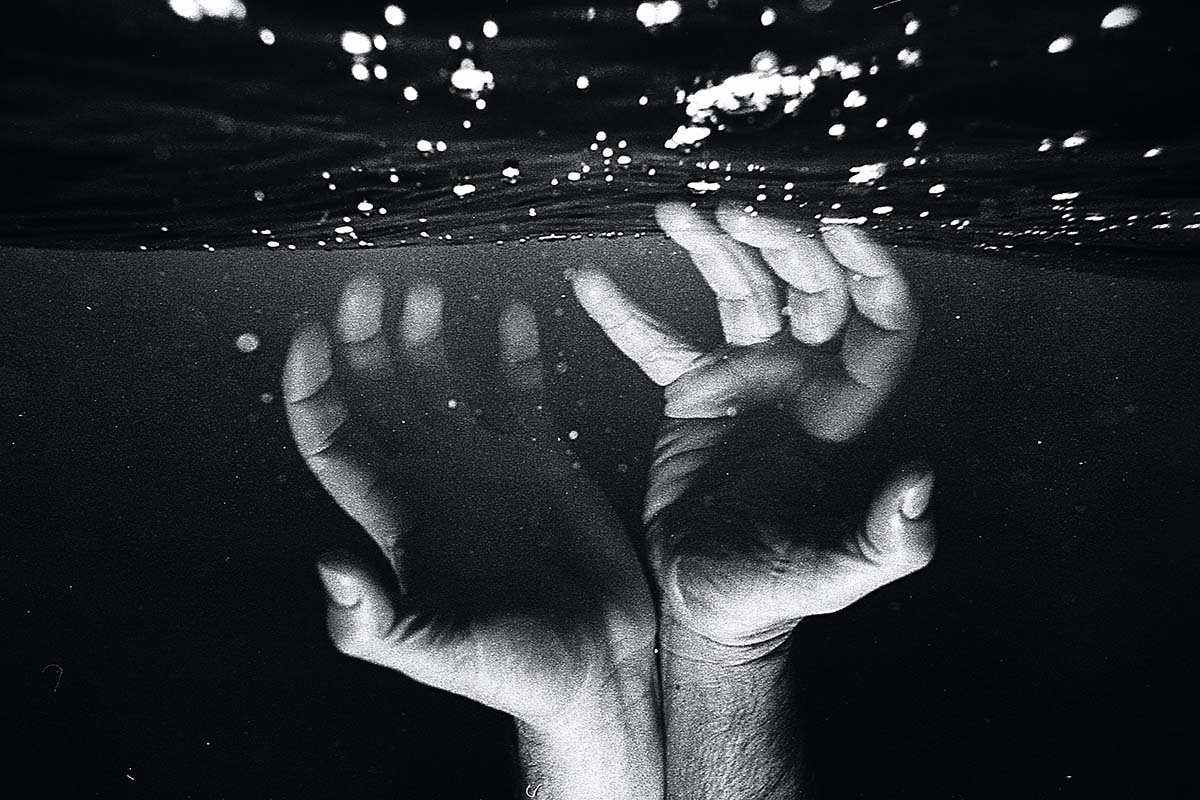
- OCD often hides behind intrusive thoughts and compulsive behaviors, making people feel ashamed or confused about what’s happening inside their mind.
- Many people with OCD go undiagnosed because symptoms overlap with anxiety, depression, and PTSD, making it harder to recognize the true disorder.
- Understanding co-occurring conditions is essential, as proper diagnosis helps reduce fear, bring clarity, and guide people toward effective treatment.
Obsessive-compulsive disorder is more than just “being neat” or “liking things a certain way.”
It’s a chronic condition where unwanted, intrusive thoughts show up again and again, creating intense anxiety that people try to quiet through repetitive actions or mental rituals.
And for many, those thoughts feel scary, embarrassing, or completely out of their control — which is why OCD often stays hidden for years.
Even though OCD affects around 2.2 million people in the U.S., a huge number remain undiagnosed.
Not because their symptoms aren’t real, but because OCD rarely shows up alone.
It often blends with other disorders, making people fear they’re “just anxious,” “overreacting,” or dealing with something much worse.
This overlap can make it tough for professionals to identify what’s actually happening, leaving people feeling misunderstood or dismissed.
Here are some of the mental health conditions that commonly occur alongside OCD — and often complicate the path to getting a clear diagnosis and the right help.
- Body Dysmorphic Disorder;
- Generalized Anxiety Disorder;
- Depression;
- Panic Disorder.
The dual diagnosis of co-occurring disorders makes OCD treatment extremely challenging.
Therefore, a medical professional must have a deep understanding of these comorbid disorders that occur alongside OCD to give a diagnosis.
Understanding and managing OCD (Obsessive-Compulsive Disorder) often requires a comprehensive approach considering linked mental health disorders.
To learn more about managing OCD effectively, it’s crucial to recognize its frequent co-occurrence with conditions like anxiety and depression.
These interconnected challenges can complicate daily life, making treatment even more vital.
Seeking help from mental health professionals who specialize in OCD and its related disorders is a crucial step.
Therapy modalities like Cognitive-Behavioral Therapy (CBT) can be immensely beneficial, equipping individuals with the tools to identify and manage obsessive thoughts and compulsive behaviors.
Furthermore, learning more about managing OCD involves building a solid support network, including friends and family who can offer understanding and encouragement along the journey to recovery.
What Is Comorbidity?
Comorbidity is when a person exhibits more than one mental health problem.
For example, if depression and anxiety are jointly diagnosed, they are referred to as comorbidities.
The co-occurring disorders are usually responsible for leading to another disorder’s development.
Therefore, medical professionals treat comorbid mental health problems simultaneously.
Disorders Related to OCD
People with OCD get diagnosed with various comorbid disorders.
Comorbid disorders differ from multiple types of OCD as those are the subtypes while these are co-occurring diseases.
Here are some common comorbid conditions that occur with OCD.
- Anxiety disorders;
- Depression;
- Post-Traumatic Stress Disorder (PTSD;)
- Eating disorders;
- Attention Deficit Hyperactivity Disorder (ADHD;)
These are typical examples of comorbid disorders that may affect how a therapist treats OCD because such conditions have overlapping symptoms.
But it is critical for a person with OCD to have the proper diagnosis for an effective treatment plan.
Similar disorders also tend to have different treatment strategies.
Thus, providing the wrong treatment for comorbid disorders can result in unnecessary suffering, wasted resources, wasted time, and hopelessness.
Now let us look into the comorbid conditions of OCD.
OCD and Panic Disorder: How They Connect and Why It Matters
OCD falls under the broader umbrella of anxiety disorders, which is why it often overlaps with conditions like panic disorder.
What many people don’t realize is that the connection between the two isn’t random — it’s rooted in how the brain responds to fear, uncertainty, and intrusive thoughts.
People with panic disorder experience sudden, intense panic attacks that feel like danger is happening right now, even when nothing is actually wrong.
The brain misreads normal sensations or thoughts as threats, which triggers a full fight-or-flight response.
For people with OCD, this can become even more complicated.
Obsessions — those intrusive, persistent thoughts — often create intense fear or discomfort.
To calm that fear, the mind develops compulsions (repeated actions or mental rituals). But when the fear spikes too quickly or feels overwhelming, it can trigger a panic attack.
This is why many people with OCD also report symptoms like:
a racing heart;
difficulty breathing;
dizziness or trembling;
a sudden sense of dread;
feeling like they’re “losing control.”
In reality, they’re experiencing a panic response to their own intrusive thoughts.
✨Understanding the link between OCD and panic disorder is incredibly helpful because it gives clarity: you’re not “going crazy,” your brain is reacting to fear it doesn’t know how to process yet.
Recognizing this pattern is often the first step in getting the right treatment — and finally breaking the cycle of fear → obsession → compulsion → panic.
OCD and Body Dysmorphic Disorder (BDD)
BDD affects the way a person sees themselves.
Even if others don’t notice anything unusual, someone with BDD may obsess over a “flaw” that feels huge, embarrassing, or impossible to ignore. This could be their skin, hair, weight, nose, or any feature they believe is “wrong.”
Because of this intense focus, people with BDD may:
check mirrors repeatedly or avoid them completely;
constantly compare themselves to others;
spend hours trying to fix or hide the perceived flaw;
seek reassurance about their appearance;
avoid social situations for fear others will notice the “problem;”
These behaviors aren’t vanity — they’re anxiety-driven and exhausting.
BDD can also influence other conditions, like eating disorders, though they are separate diagnoses. Understanding the difference helps people get the right support.
If any of this sounds familiar, here are a few helpful steps:
Notice patterns: When do you start checking or avoiding?
Limit reassurance-seeking: It often makes anxiety worse long-term.
Talk to a professional: BDD responds well to CBT and specific OCD-focused treatments.
Be kind to yourself: This is a medical condition, not a personal failure.
The key is recognizing that BDD isn’t about flaws — it’s about fear
. And once you understand that, it becomes easier to take steps toward feeling better and getting the right help.
OCD’s Relationship With Anxiety Disorders
Anxiety is often a co-occurring disorder. Generalized anxiety disorder, panic attacks, and phobias often co-occur.
Moreover, anxiety disorder is the most common co-occurring disorder of OCD.
Anxiety symptoms are variable, but they make a patient worried and nervous.
Patients may feel that their worries and nervousness are illogical.
But they subconsciously affect an individual to the point that it starts deteriorating their physical health.
Some notable anxiety symptoms are hand tremors, sweaty palms, nervousness, jitteriness, etc.
Even if an individual recognizes anxiety symptoms, they cannot treat the negative thoughts without seeking medical assistance.
OCD and Linked Mental Health Disorders: OCD and Mood Disorders
Mood disorder is commonly used to describe various types of depression, such as the following.
- Postpartum depression;
- Major depression;
- Bipolar disorder;
- Chronic depression.
The symptoms and triggers of mood disorders differ for every individual as it exclusively depends on the type of mood disorder and the severity of the problem.
Here are some of the common symptoms.
- Disinterest in activities;
- Low mood;
- Extreme mood fluctuations;
- Thoughts of self-harm/suicide;
- Feeling helpless;
- Negative feelings about self.
OCD and Major Depressive Disorder
Major depressive disorder often coexists with OCD.
These two mental health disorders feed off each other and grow more severe.
It doesn’t matter which of the two mental health disorders occurs first.
Obsessive-compulsive disorder can make a person feel hopeless and stuck. It also significantly affects their self-esteem.
Such feelings can give rise to major depressive disorder.
Therefore, OCD and major depressive disorder often have common symptoms, making it challenging to identify the two conditions separately.
Moreover, you’d be surprised to know that depressive disorders correlate with the imbalance of our brain chemicals called serotonin.
A chemical imbalance of serotonin also results in OCD.
Therefore, these are closely related mental health disorders that affect an individual’s self-esteem and feelings.
OCD and Eating Disorders
Some people with OCD may have an obsession and compulsion related to food. This creates various eating disorders, such as the following.
- Binge eating disorder;
- Bulimia;
- Anorexia nervosa.
While these disorders significantly differ, they result from obsessiveness and compulsivity.
For example, a common factor is a person’s obsession with food.
People with an eating disorder often obsess over their eating habits and feel anxious when they do not follow a specific pattern.
If a person with OCD develops a compulsiveness regarding food, they must closely inspect their eating behavior as there is a high risk of developing an eating disorder.
OCD and Self Harm
Anyone with intrusive thoughts about suicide and self-harm should seek professional medical help.
In addition, people with OCD must monitor their conditions for signs of anxiety and depression, as these comorbidities can worsen intrusive thoughts.
About 60% of people with OCD experience one depressive episode. Such episodes can worsen intrusive thoughts.
Besides this, bipolar disorder can also contribute to manic periods.
Such people are also more likely to develop OCD.
OCD and Linked Mental Health Disorders: Final Words
Various other comorbidities can occur with OCD.
But the comorbidities mentioned above are the most common disorders with OCD, making it challenging for medical healthcare providers to identify them.
Professional treatment is vital for someone who experiences OCD and associated disorders before the symptoms worsen.
But treatment isn’t the only piece of the puzzle when it comes to managing OCD.
A big part of the work happens in everyday moments — especially when you’re dealing with hesitation, avoidance, or that familiar pull to “do it later.”
Understanding why we procrastinate is actually a huge part of OCD recovery, because procrastination often comes from fear, uncertainty, or the urge to avoid uncomfortable thoughts.
And the more we avoid, the stronger the compulsions become.
That’s why learning to build small habits of self-control and reducing indecisiveness matters so much.
Every time you resist a compulsion or take a tiny step forward instead of delaying it, you weaken the OCD cycle.
Recovery isn’t about forcing yourself to change overnight — it’s gradual, step-by-step progress, and patience is a major part of the process.
OCD may be chronic, but it is absolutely treatable, and many people get significantly better when they understand their patterns and stay committed to improving.
With the right support, knowledge, and consistent effort, you can retrain your mind and reclaim a sense of calm and control.